2019-10-26 农历九月二十八
每天精选一篇文献,陪你度过2019的365天
知识城邦,从临床医生视角,分享解读最前沿最实用的文献
(总第306篇)
不要憎恨你的敌人,那会影响你的判断——《教父》


内镜下实时人工智能检测上消化道肿瘤:一项多中心病例对照的诊断性研究
—结论—
人工智能系统GRAIDS对诊断上消化道肿瘤具有高准确率,其敏感性与内镜专家相似,优于非内镜专家。该系统可以帮助社区医院提高上消化道肿瘤的诊断效能。
GRAIDS achieved high diagnostic accuracy in detecting upper gastrointestinal cancers, with sensitivity similar to that of expert endoscopists and was superior to that of non-expert endoscopists. This system could assist community-based hospitals in improving their effectiveness in upper gastrointestinal cancer diagnoses.—背景—
上消化道肿瘤(包括食管癌和胃癌)是世界上最常见的肿瘤。使用深度学习算法的人工智能平台在医学影像方面取得了重大进展,但其在上消化道肿瘤中的应用仍受到限制。我们希望通过对临床内镜图像资料的分析,建立并验证胃肠道人工智能诊断系统(GRAIDS),用于诊断上消化道肿瘤。
Upper gastrointestinal cancers (including oesophageal cancer and gastric cancer) are the most common cancers worldwide. Artificial intelligence platforms using deep learning algorithms have made remarkable progress in medical imaging but their application in upper gastrointestinal cancers has been limited. We aimed to develop and validate the Gastrointestinal Artificial Intelligence Diagnostic System (GRAIDS) for the diagnosis of upper gastrointestinal cancers through analysis of imaging data from clinical endoscopies.—方法—
这项多中心、病例对照的诊断性研究在中国的6家不同级别的医院(市、省和国家)进行。
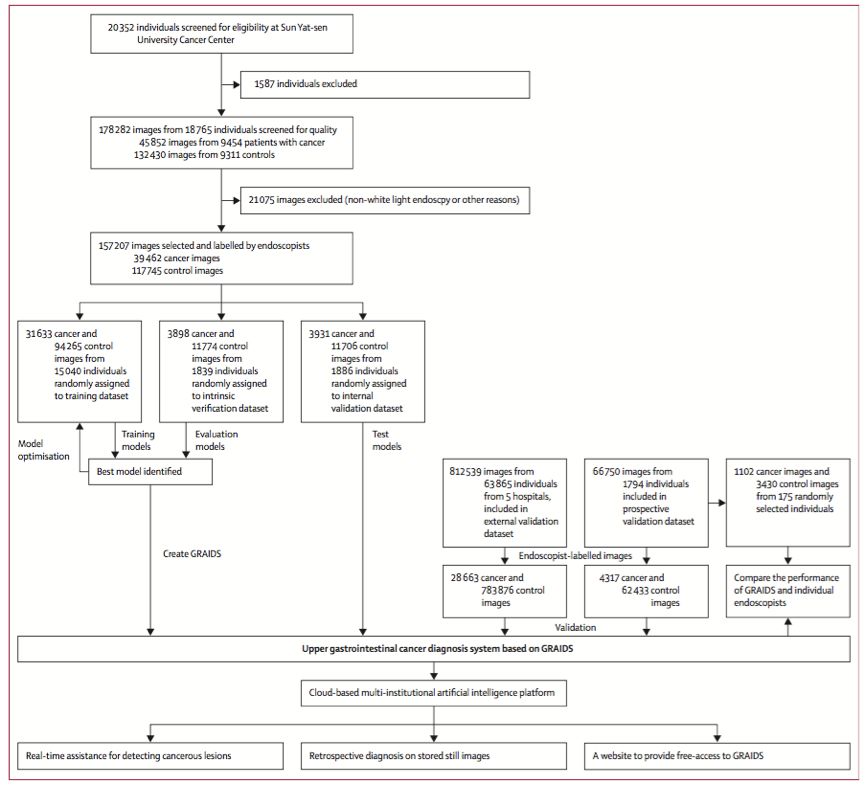
从所有参与医院中纳入18岁或18岁以上既往未进行过内镜检查的患者连续的内镜图像。所有经组织学证实为上消化道恶性肿瘤的患者(包括食管癌和胃癌)均符合本研究的要求。只有带有标准白光的图像才被认为是合格的。
将中山大学肿瘤中心的图像随机(8:1:1)分配到开发GRAIDS的训练和内部验证数据集以及评估GRAIDS性能的内部验证数据集。采用中山大学肿瘤中心的内部和前瞻性验证集及5家基层医院的外部验证集对其诊断性能进行评估。GRAIDS的性能也与三个专业级别的内镜医师进行了比较:专家、主治医师和实习医师。
采用氯珀-皮尔逊法计算95%顺式积分以评估GRAIDS和内镜医师对肿瘤病变的诊断准确度、敏感性、特异性、阳性预测值和阴性预测值。。
This multicentre, case-control, diagnostic study was done in six hospitals of different tiers (ie, municipal, provincial, and national) in China. The images of consecutive participants, aged 18 years or older, who had not had a previous endoscopy were retrieved from all participating hospitals. All patients with upper gastrointestinal cancer lesions (including oesophageal cancer and gastric cancer) that were histologically proven malignancies were eligible for this study. Only images with standard white light were deemed eligible. The images from Sun Yat-sen University Cancer Center were randomly assigned (8:1:1) to the training and intrinsic verification datasets for developing GRAIDS, and the internal validation dataset for evaluating the performance of GRAIDS. Its diagnostic performance was evaluated using an internal and prospective validation set from Sun Yat-sen University Cancer Center (a national hospital) and additional external validation sets from five primary care hospitals. The performance of GRAIDS was also compared with endoscopists with three degrees of expertise: expert, competent, and trainee. The diagnostic accuracy, sensitivity, specificity, positive predictive value, and negative predictive value of GRAIDS and endoscopists for the identification of cancerous lesions were evaluated by calculating the 95% CIs using the Clopper-Pearson method.
—结果—
用1 036 496张来自84 424名患者的内窥镜图像来开发和测试GRAIDS。
上消化道肿瘤的诊断准确率在内部验证集中为0.955(95%CI: 0.952-0.957),在前瞻性验证集中为0.927(0.925-0.929),在5个外部验证集中为0.915(0.913-0.917)到0.977(0.977-0.978)之间。
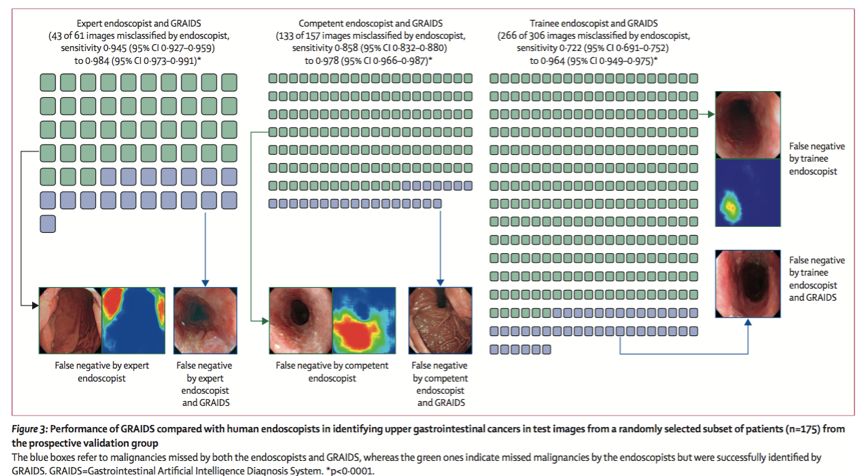
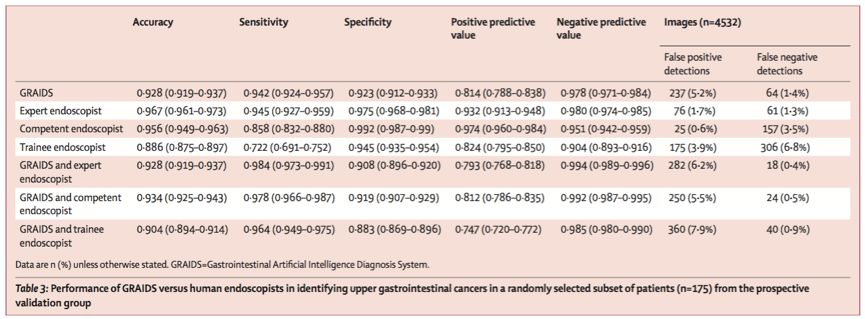
GRAIDS的诊断敏感性与内镜专家(0.942[95%CI: 0.924-0.957] vs 0.945[0.927-0.959]; p=0.692)相似,与内镜主治医师(0.858[0.832-0.880], p<0.0001)和实习医生(0.722[0.691-0.752], p<0.0001)相比,GRAIDS具有更高的敏感性。
GRAIDS的阳性预测值为0.814(95%CI: 0.788-0.838),内镜专家为0.932(0.913-0.948),内镜主治医师为0.974(0.960-0.984),实习医生为0.824(0.795-0.850)。GRAIDS阴性预测值为0.978(95%cCI: 0.971-0.984),内镜专家阴性预测值为0.980(0.974-0.985),内镜主治医师阴性预测值为0.951(0.942-0.959),内镜实习医生阴性预测值为0.904(0.893-0.916)。
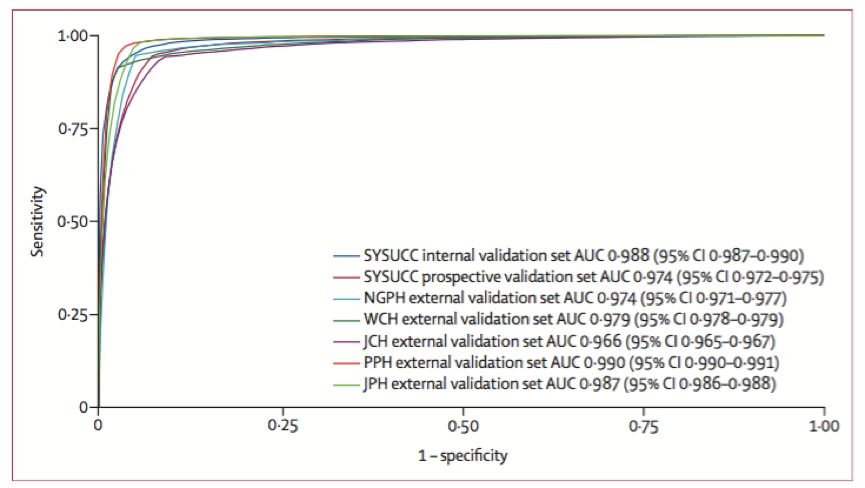
1?036?496 endoscopy images from 84?424 individuals were used to develop and test GRAIDS. The diagnostic accuracy in identifying upper gastrointestinal cancers was 0·955 (95% CI 0·952–0·957) in the internal validation set, 0·927 (0·925–0·929) in the prospective set, and ranged from 0·915 (0·913–0·917) to 0·977 (0·977–0·978) in the five external validation sets. GRAIDS achieved diagnostic sensitivity similar to that of the expert endoscopist (0·942 [95% CI 0·924–0·957] vs 0·945 [0·927–0·959]; p=0·692) and superior sensitivity compared with competent (0·858 [0·832–0·880], p<0·0001) and trainee (0·722 [0·691–0·752], p<0·0001) endoscopists. The positive predictive value was 0·814 (95% CI 0·788–0·838) for GRAIDS, 0·932 (0·913–0·948) for the expert endoscopist, 0·974 (0·960–0·984) for the competent endoscopist, and 0·824 (0·795–0·850) for the trainee endoscopist. The negative predictive value was 0·978 (95% CI 0·971–0·984) for GRAIDS, 0·980 (0·974–0·985) for the expert endoscopist, 0·951 (0·942–0·959) for the competent endoscopist, and 0·904 (0·893–0·916) for the trainee endoscopist.
—附图—
分享者| SOA
编辑:SOA
美术设计:SOA
?知识城邦 苟日新,日日新
查看或下载文献原文,点击左下角“阅读原文